PC4/PAC3 2022 Spring Conference Posters
Welcome to the 2022 Spring Conference Virtual Poster Session!
The authors recorded brief descriptions to enhance their presentation; click the “Download” button and “Play Slide Show” to listen to the description. Email the primary author with any questions or comments by clicking on their name below the poster.
[one_half]
Reduction of Duration of a Fat-Modified Diet for Chylothorax: Success at two centers
Jason Buckley, MD Medical University of South Carolina
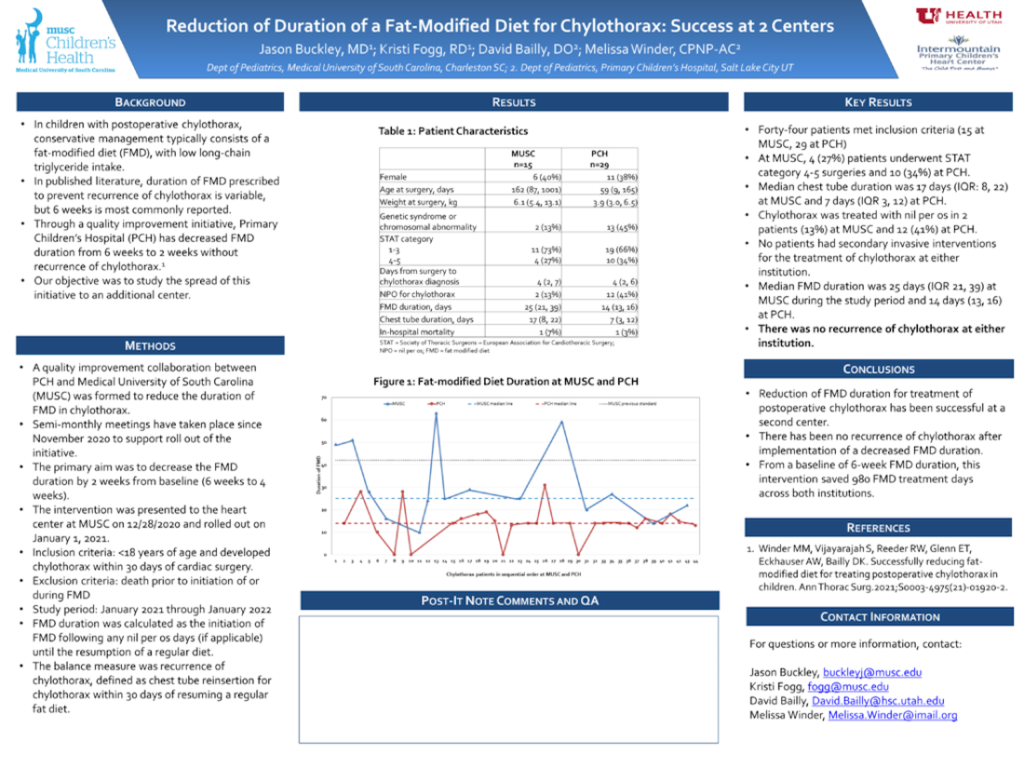
[/one_half] [one_half_last]A comprehensive closed loop debriefing program to improve patient outcomes and code team performance
Kimberly DiMaria, CPNP-AC, CCRN Children’s Hospital Colorado
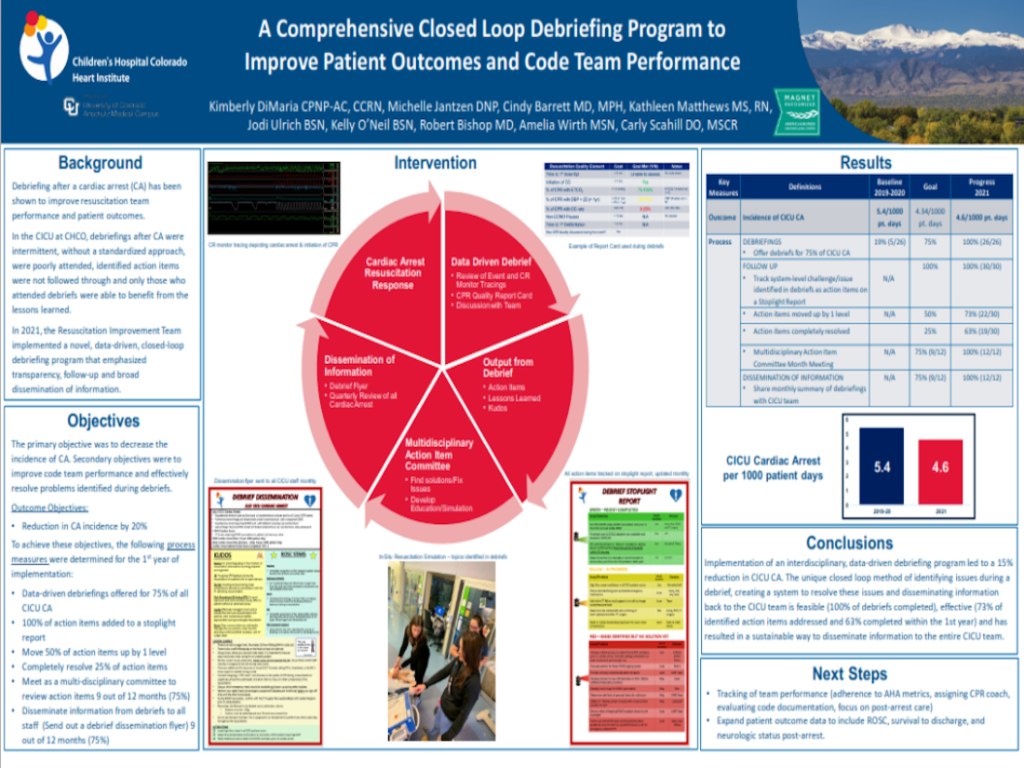
[/one_half_last] [one_half]Escalation of care bundle improves outcomes in the Cardiac Progressive Care Unit
Kimberly DiMaria, CPNP-AC, CCRN Children’s Hospital Colorado
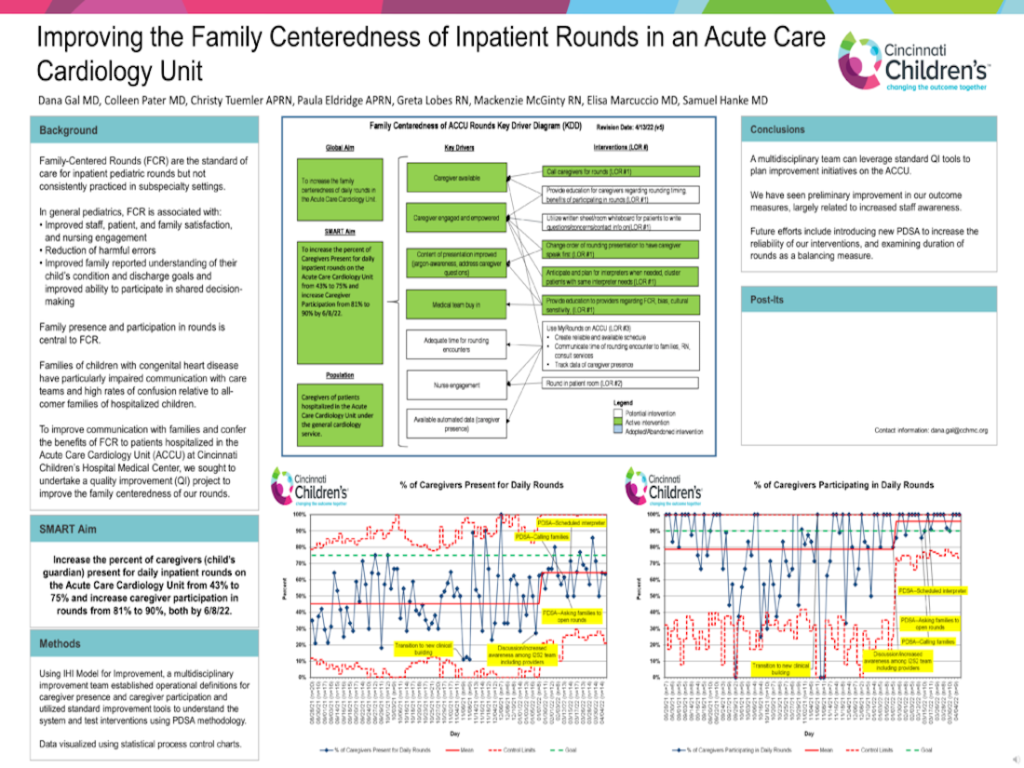
[/one_half] [one_half_last]Improving the family centeredness of inpatient rounds in an Acute Care Cardiology unit
Dana Gal, MD Cincinnati Children’s Hospital
[/one_half_last] [one_half]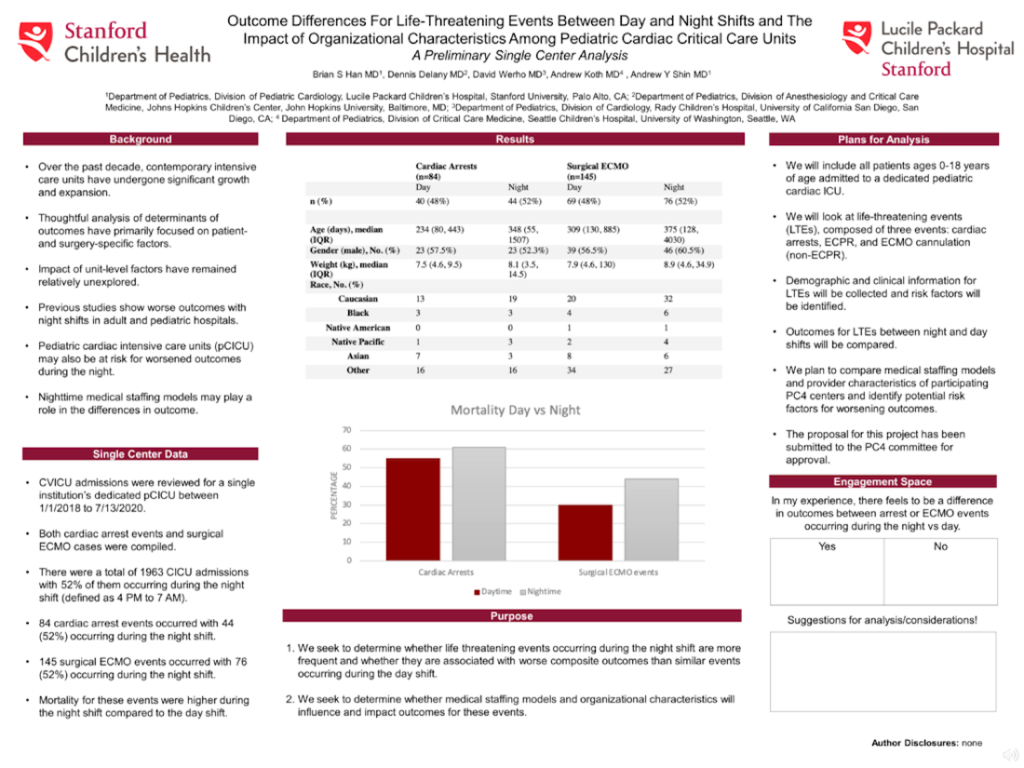
Outcome differences for life-threatening events between day and night shifts and the impact of organizational characteristics among Pediatric Cardiac Critical Care Units: A preliminary single center analysis
Brian Han, MD Lucile Packard Children’s Hospital at Stanford
[/one_half] [one_half_last]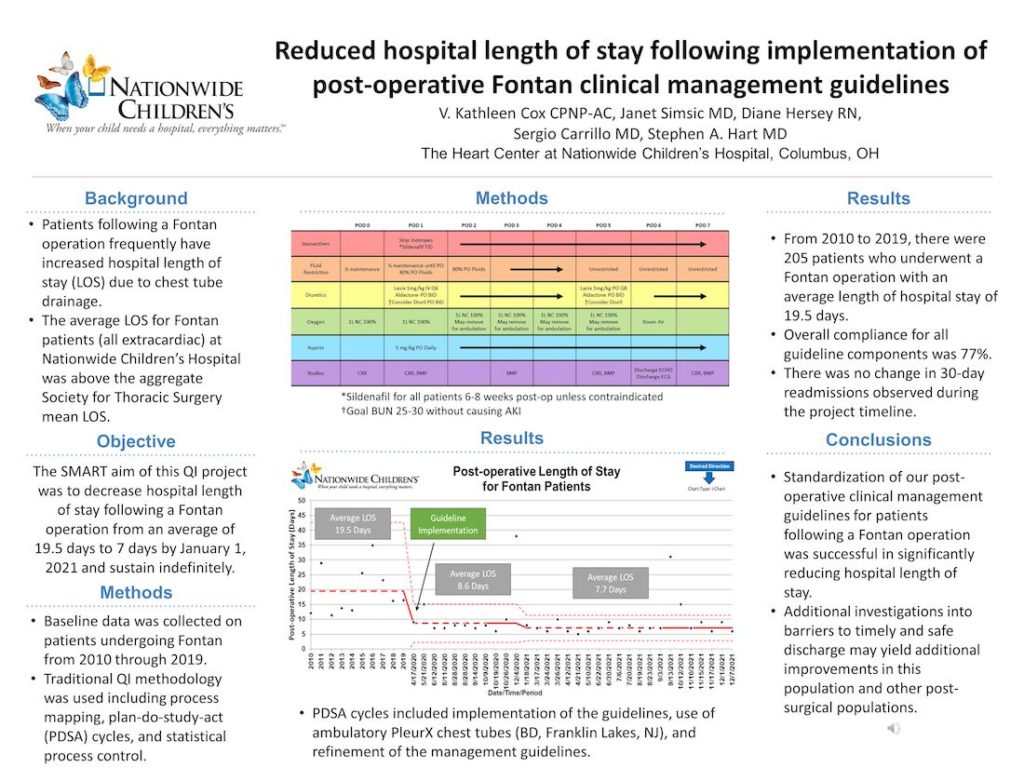
Reduced hospital length of stay following implementation of post-operative Fontan clinical management guidelines
Stephen Hart, MD Nationwide Children’s Hospital
[/one_half_last] [one_half]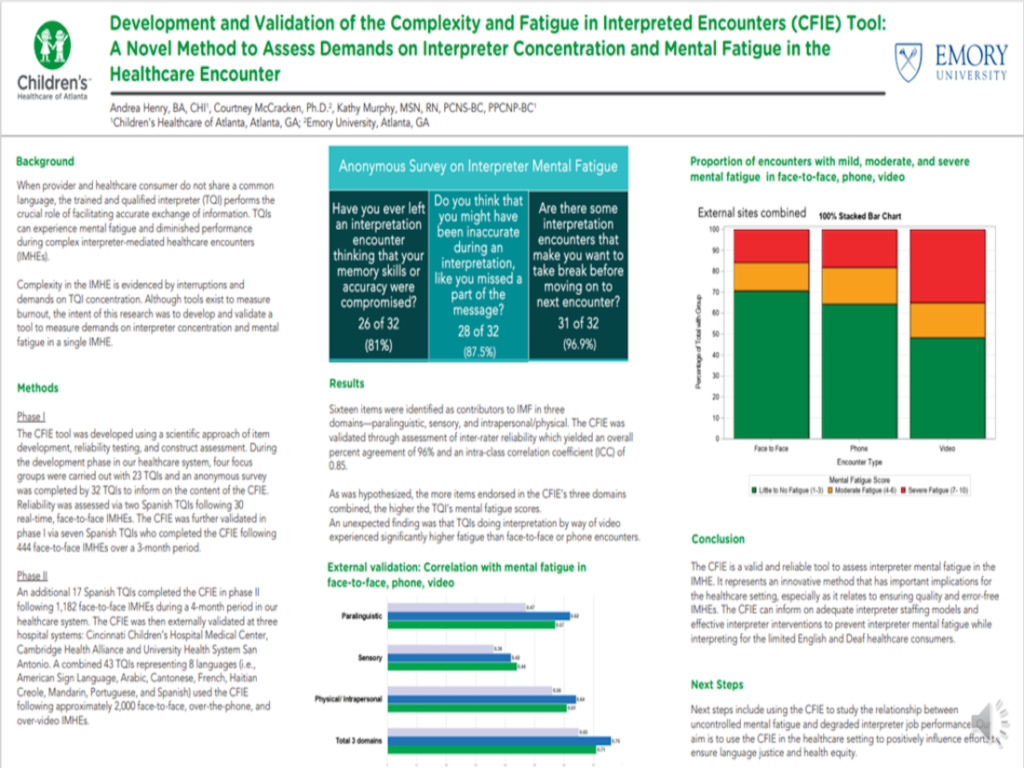
Development and validation of the Complexity and Fatigue in Interpreted Encounters (CFIE) Tool: A novel method to assess demands on interpreter concentration and mental fatigue in the healthcare encounter
Andrea Henry, BA, CHI Children’s Healthcare of Atlanta
[/one_half] [one_half_last]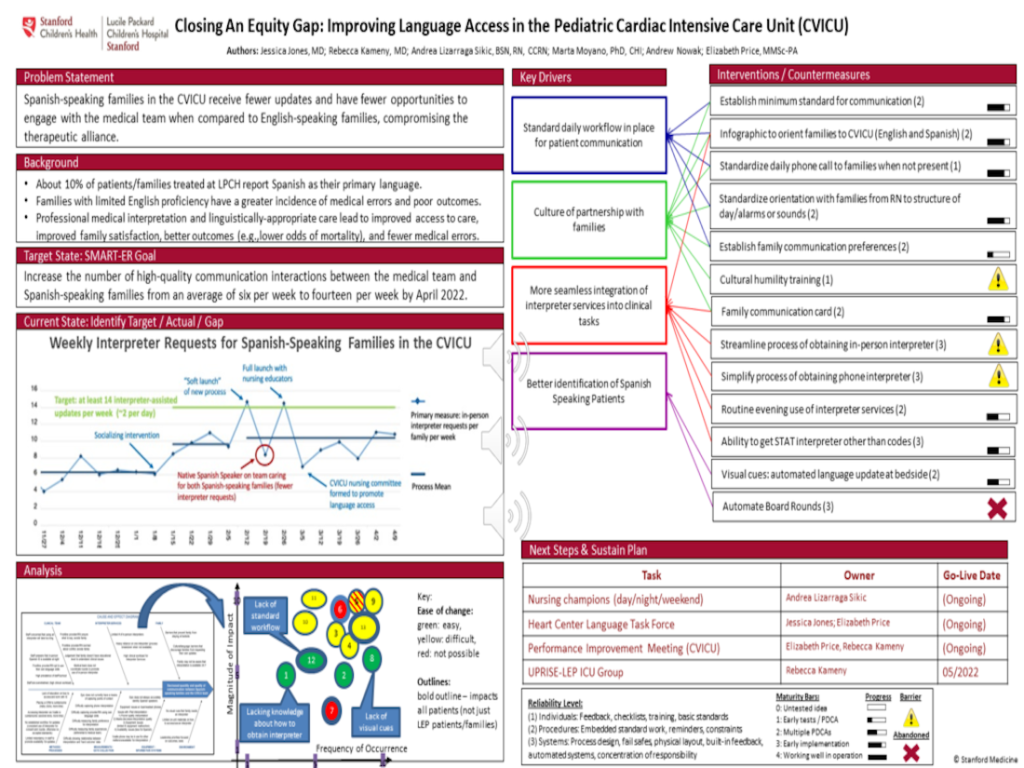
Closing an equity gap: Improving language access in the Pediatric Cardiac Intensive Care Unit (CVICU)
Jessica Jones, MD Lucile Packard Children’s Hospital at Stanford
[/one_half_last] [one_half]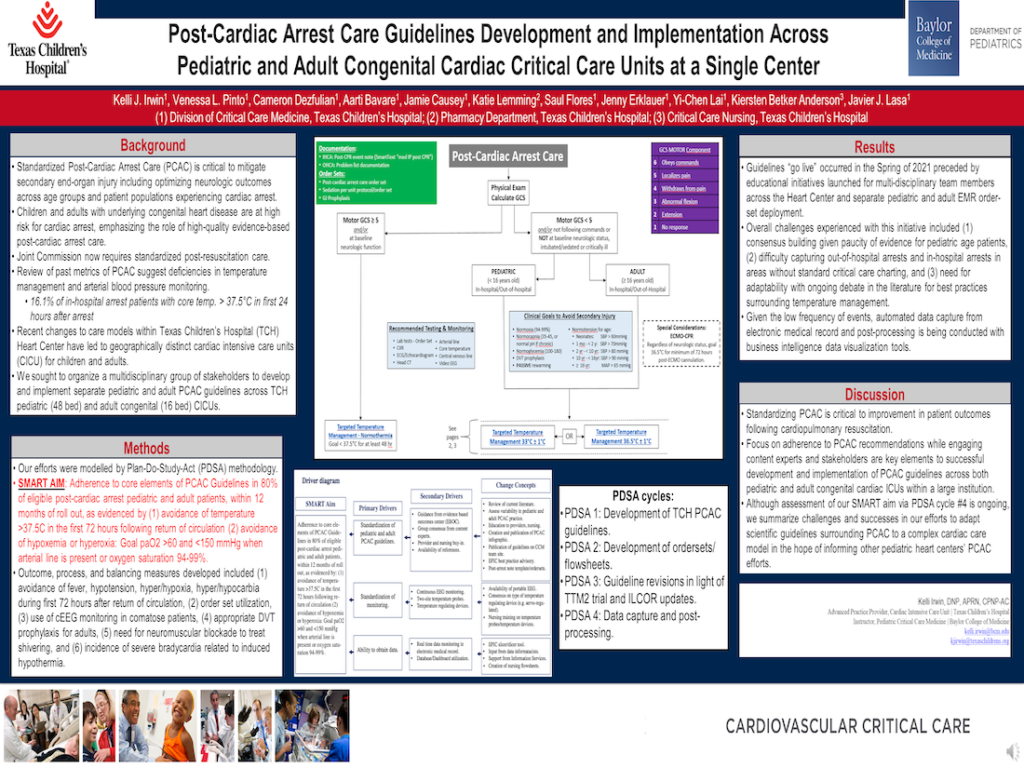
Post-Cardiac Arrest Care Guidelines Development and Implementation Across Pediatric and Adult Congenital Cardiac Critical Care Units at a Single Center
Kelli Irwin, DNP, APRN, CPNP-AC Texas Children’s Hospital
[/one_half] [one_half_last]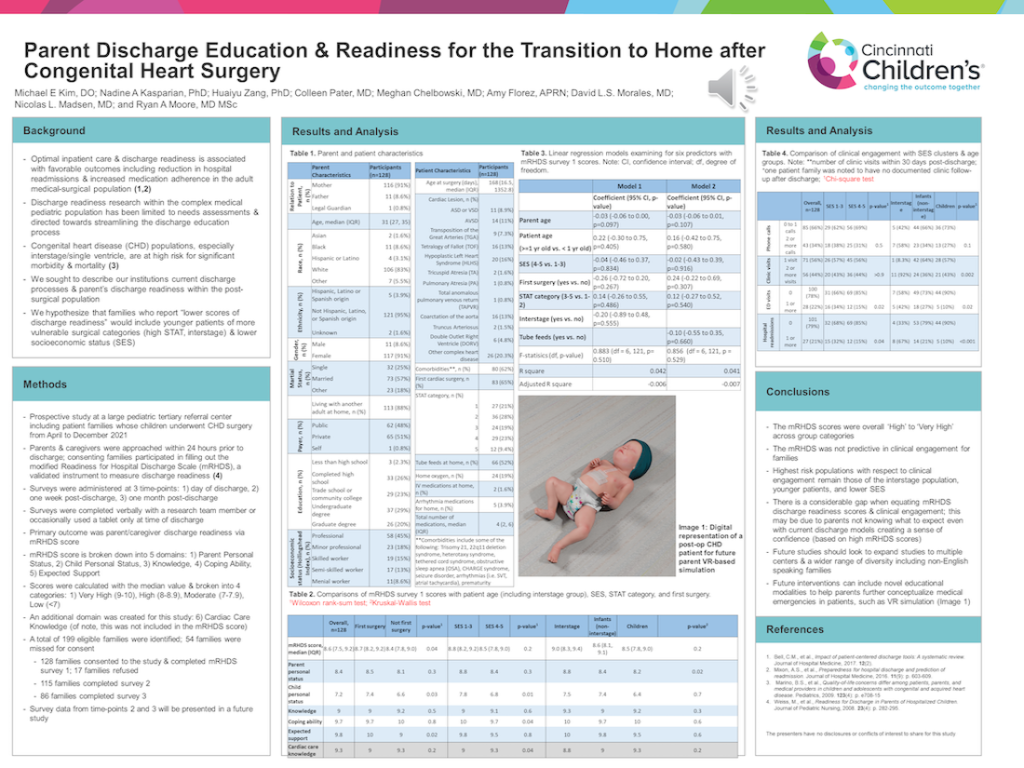
Parent discharge education & readiness for the transition to home after congenital heart surgery
Michael Kim, DO Cincinnati Children’s Hospital
[/one_half_last] [one_half]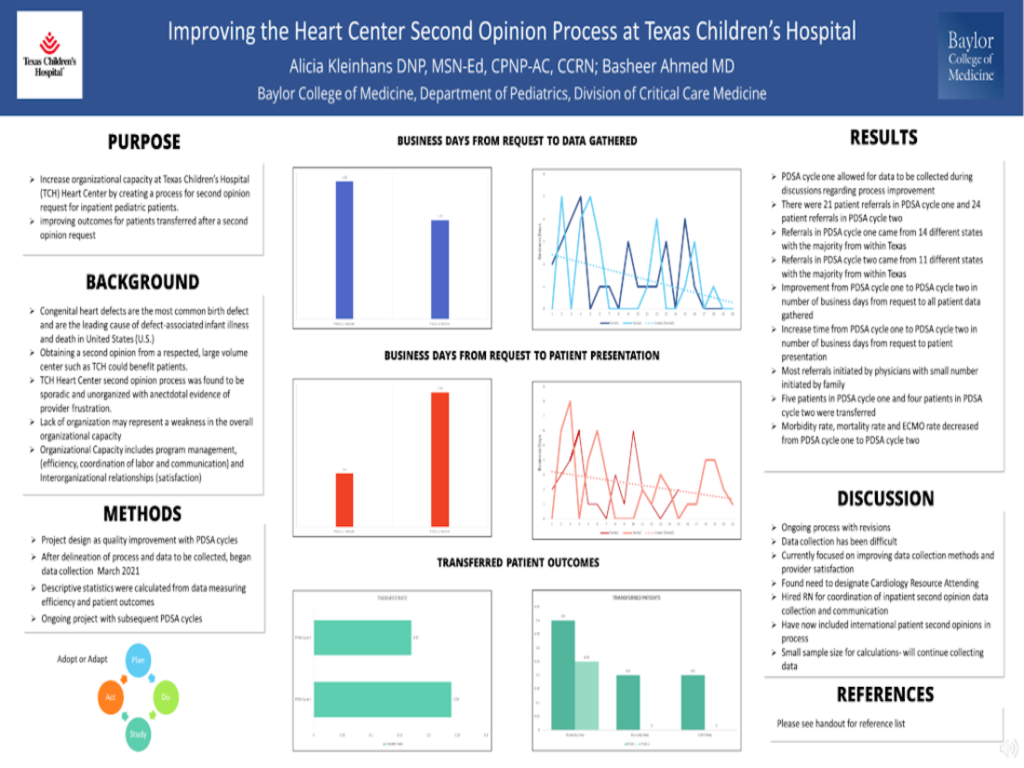
Improving the Heart Center second opinion process at Texas Children’s Hospital
Alicia Kleinhans, DNP, MSN-Ed, CPNP-AC, CCRN Texas Children’s Hospital
[/one_half] [one_half_last]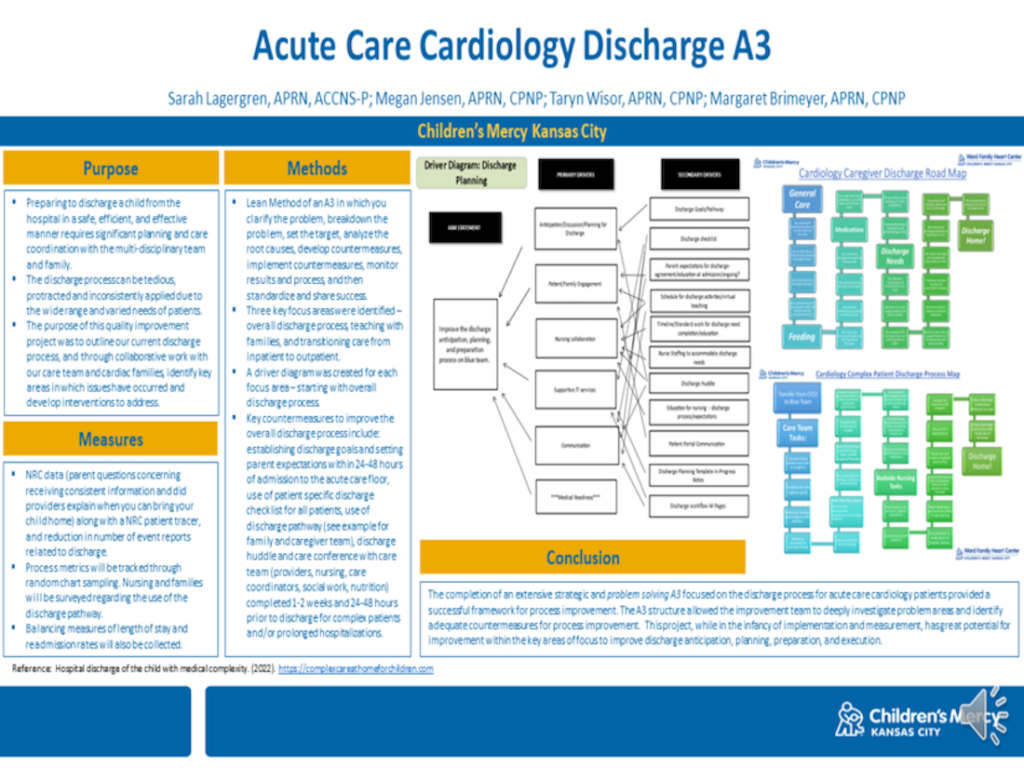
Children’s Mercy Hospital: Acute Care Cardiology Discharge A3
Sarah Lagergren, APRN, ACCNS-P Children’s Mercy Hospital, Kansas City
[/one_half_last] [one_half]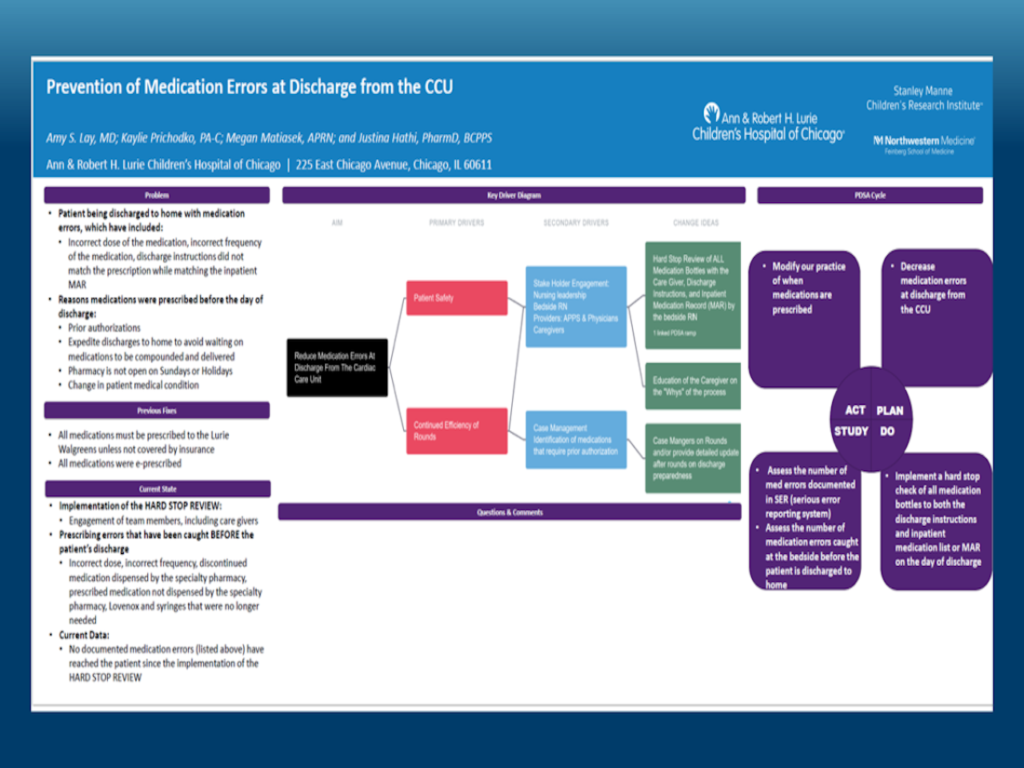
Prevention of Medication Errors at Discharge from the CCU
Amy Lay, MD Ann & Robert H. Lurie Children’s Hospital of Chicago
[/one_half] [one_half_last]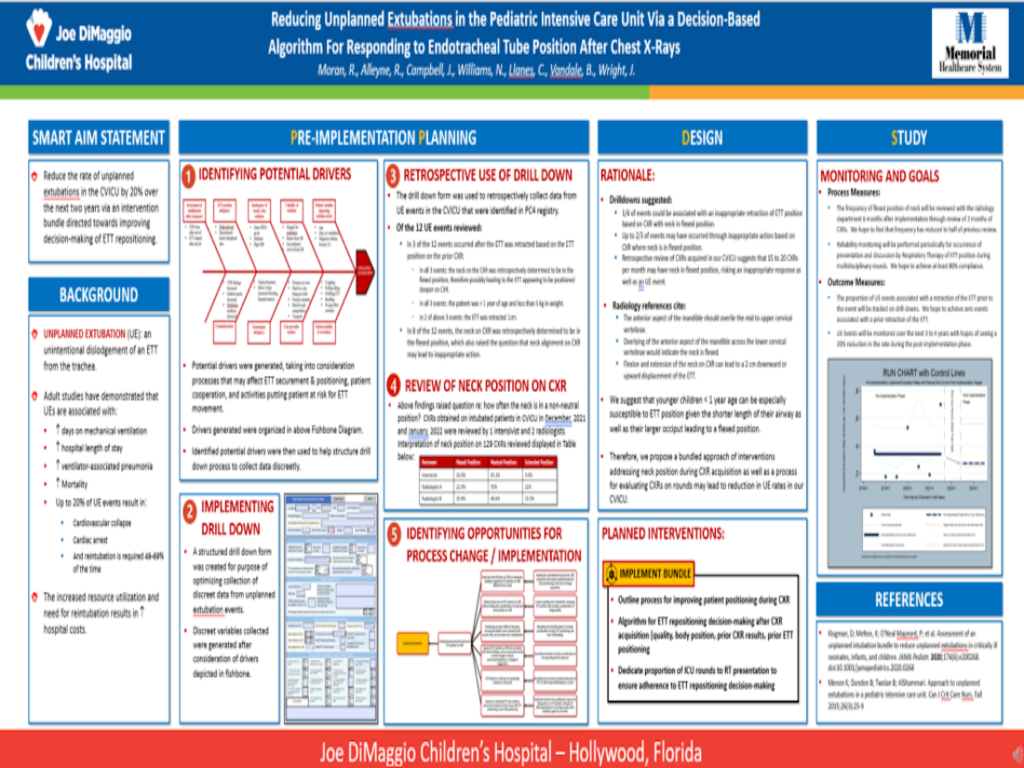
Reducing unplanned extubations in the Pediatric Intensive Care Unit via a decision-based algorithm for responding to Endotracheal tube position after chest x-rays
Ryan Moran, MD Memorial Healthcare System, Joe DiMaggio Children’s Hospital
[/one_half_last] [one_half]
Reducing unnecessary prescriptions at the time of discharge
Martha Nicholson, MD Lucile Packard Children’s Hospital at Stanford
[/one_half] [one_half_last]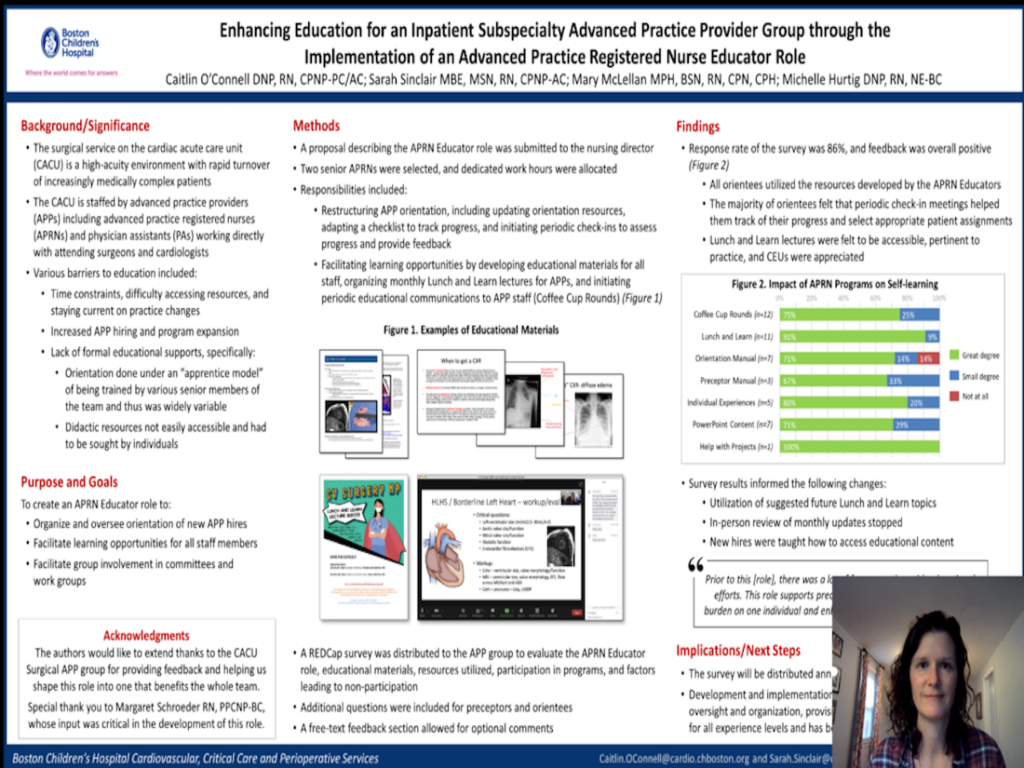
Enhancing Education for an Inpatient Subspecialty Advanced Practice Provider Group through the Implementation of an Advanced Practice Registered Nurse Educator Role
Caitlin O’Connell, DNP, RN, CPNP-PC/AC Boston Children’s Hospital
[/one_half_last] [one_half]
A single center perspective on standardized practices for Central Venous Catheter removal in Acute Care Cardiology
Megan Rodts, MD Cincinnati Children’s Hospital
[/one_half] [one_half_last]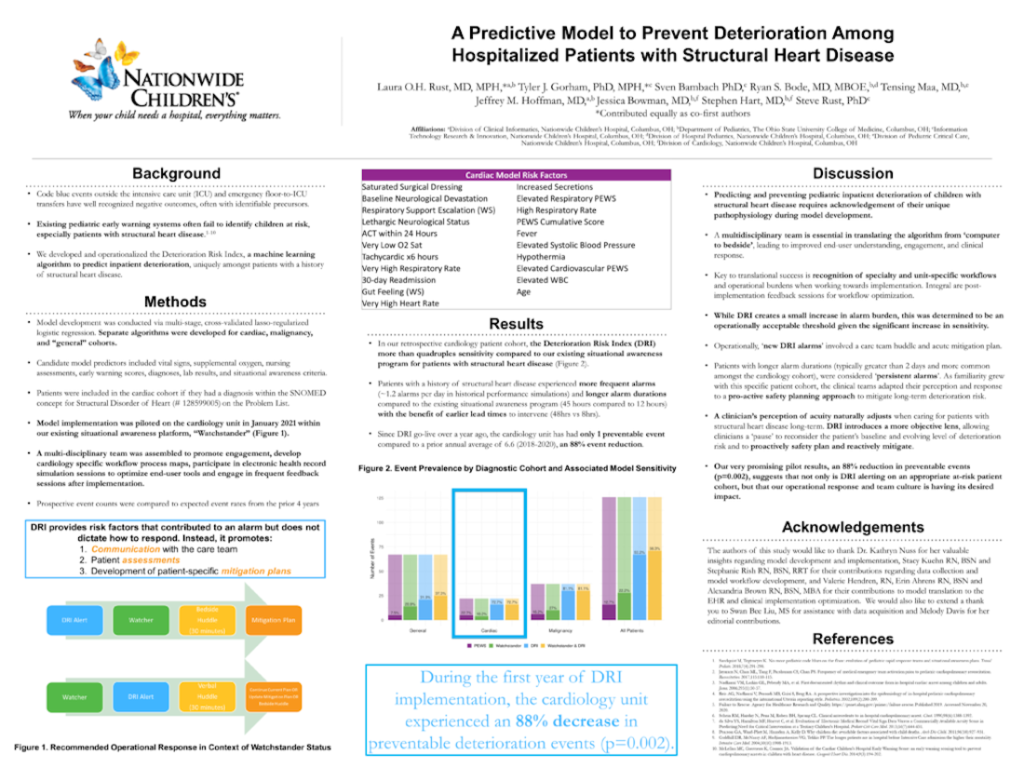
A predictive model to prevent deterioration among hospitalized patients with structural heart disease
Laura Rust, MD, MPH Nationwide Children’s Hospital
[/one_half_last] [one_half]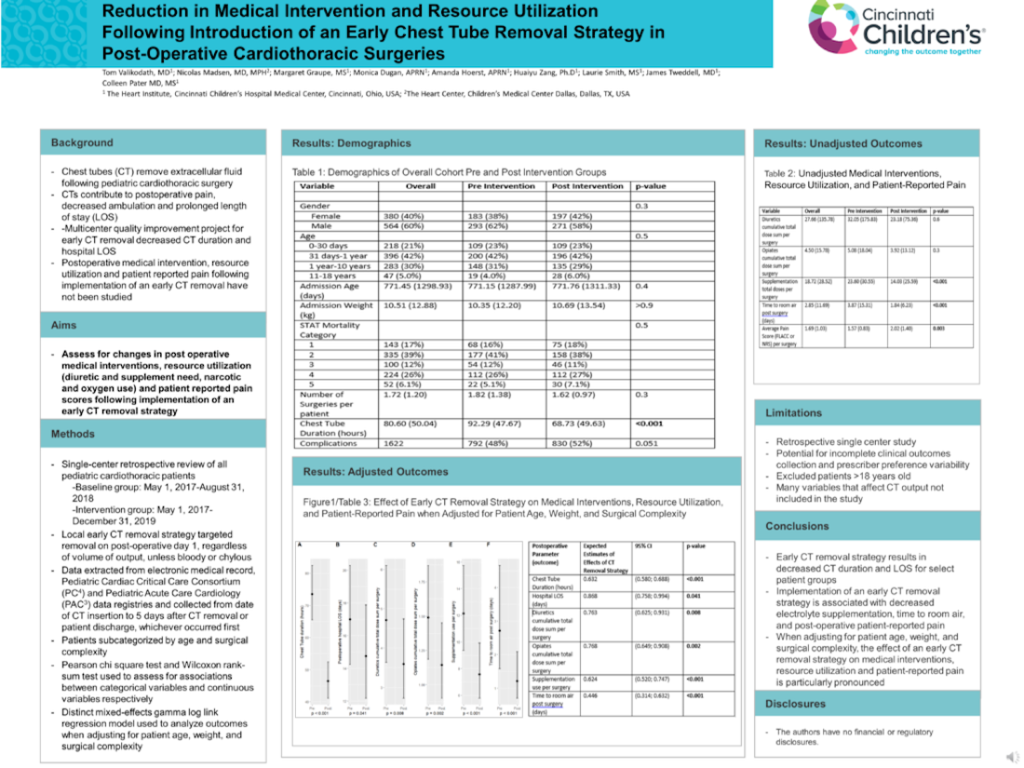
Reduction in medical intervention and resource utilization following introduction of an early chest tube removal strategy in post-operative cardiothoracic surgeries
Tom Valikodath, MD Cincinnati Children’s Hospital
[/one_half] [one_half_last]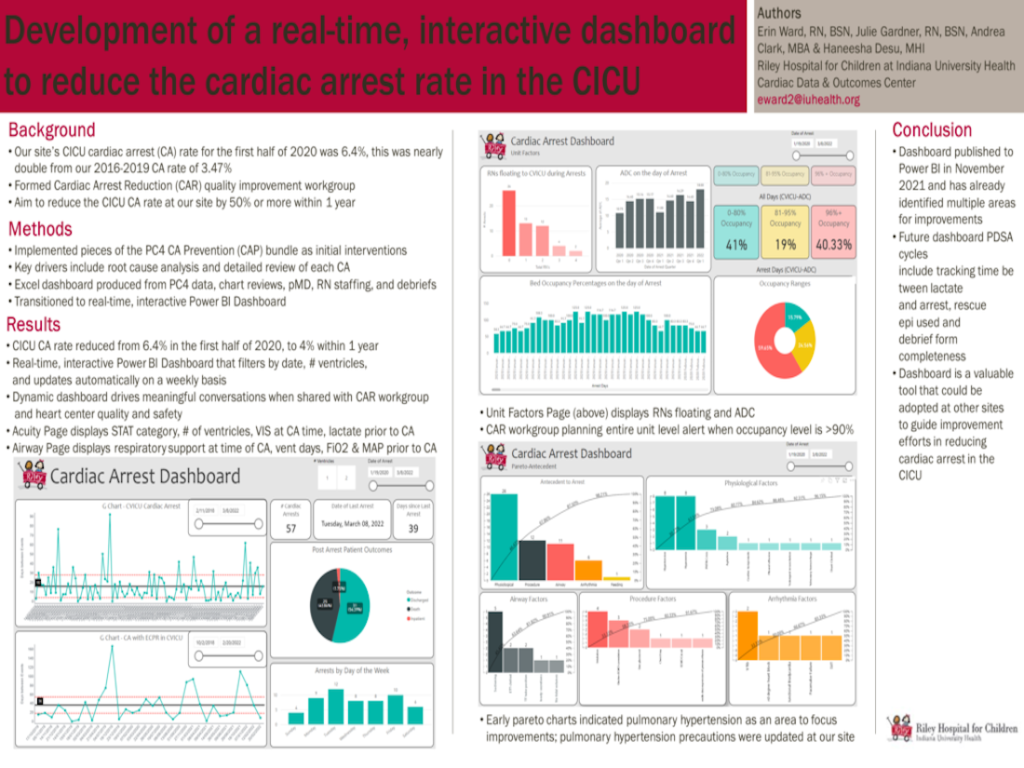
Development of a real-time, interactive dashboard to reduce the cardiac arrest rate in the CICU
Erin Ward, RN, BSN Riley Hospital for Children, Indiana University Health
[/one_half_last] [one_half]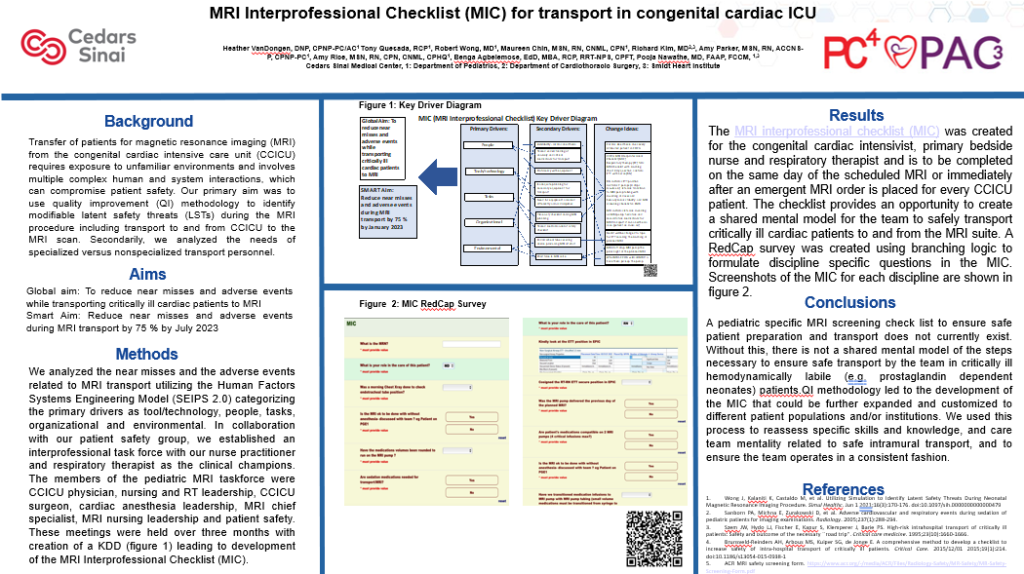
MRI Interprofessional Checklist (MIC) for transport in congenital cardiac ICU
Pooja Nawathe, MD, FAAP, FCCM Cedars Sinai Medical Center
[/one_half] [one_half_last]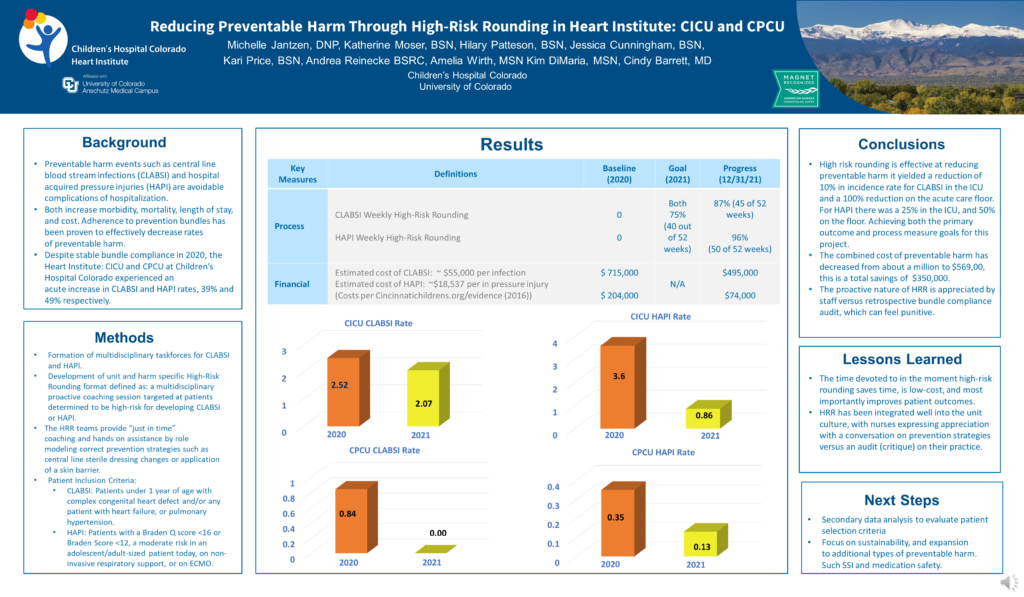
Reducing Preventable Harm Through High-Risk Rounding in Heart Institute: CICU and CPCU
Michelle Jantzen, DNP Children’s Hospital Colorado
[/one_half_last]